Unlock Higher Revenue with AI in Medical Billing And Coding
- TECHVIFY Team
- 0 Comments
Today, it’s nearly impossible to imagine a medical facility managing its revenue cycle without some form of software. And if we’re being honest, we’d wager that medical billers and coders, the unsung heroes of revenue cycle management have plenty to say about the strengths and weaknesses of those systems.
Let’s face it: software can be frustrating. It’s not perfect, and we don’t always get the seamless workflows we dream of. But here’s the good news: AI in medical billing and AI in medical coding are stepping in to fill those gaps. With these tools, we’re not just patching up inefficiencies—we’re building smarter, faster, and more reliable systems to help billers and coders thrive.
That’s what we’re diving into today: how AI is changing the game for medical coding and billing. If you’re sensing that the timing is perfect for this kind of innovation, you’re absolutely right. What you need now is the nitty-gritty—how it works, why it matters, and what’s in it for you. Let’s take that step together.
TL;DR: AI reduces errors in medical billing by automating repetitive tasks, predicting claim risks, and learning from past denials. It streamlines insurance checks, accelerates claims submissions, and ensures more accurate coding, leading to higher revenue and reduced staff burnout.
I. The Decline of Paper-Based Claim-to-Payment Processes
Let’s take a moment to reflect on the not-so-distant past when healthcare providers had to navigate the cumbersome world of paper-based billing and claims. Surprisingly, as recently as 2017, 77% of physician practices were still using paper-backed processes for billing. While more recent statistics are hard to come by, even if that percentage has dropped to somewhere between 40–50%, that’s still an overwhelming number of providers relying on outdated workflows.
AI medical billing
For those who have experienced it, the challenges of a paper-based system are all too familiar:
- Collecting data for claims
- Preparing and submitting claims
- Managing denials
- Recording payments
Now imagine doing all of that manually, with the added delay of mail delivery services. It’s no wonder healthcare providers describe this process as a nightmare. Given the strict deadlines for claim submissions imposed by carriers, paper workflows are often a recipe for disaster.
Fortunately, AI-driven medical billing systems, like GaleAI, are revolutionizing this space. By automating tedious, time-consuming tasks, these solutions allow healthcare providers to process claims with remarkable speed and accuracy, dramatically reducing the need for manual intervention. And while simply digitizing workflows is a game-changer, the next step—AI and machine learning (ML)-driven data processing—offers even greater promise.
If you’re a provider still relying on paper workflows, it’s time to explore solutions like GaleAI. The efficiency of AI-powered coding and billing will leave you amazed, simplifying revenue cycle management in ways that would have been unimaginable just a decade ago. In today’s healthcare landscape, this is no longer optional—it’s essential.
II. AI’s Transformative Role in Medical Billing and Coding
Now that we’ve recognized the challenges of traditional workflows, let’s explore the transformative role of AI in medical billing and coding.
AI in Medical Coding
The introduction of AI medical coding software has revolutionized how coding processes are handled. Let’s break it down:
-
Automated Data Recognition
AI excels at parsing through digital documentation, such as patient records, doctor notes, and medical reports, with unmatched precision. Additionally, it can analyze professional imagery, like scans or X-rays, and convert handwritten notes into digital text using optical character recognition (OCR). This makes even paper-based records accessible for training smart algorithms. -
Allowing Different Applications of AI in Coding
The applications of AI in medical coding are flexible and powerful. For instance, real-time feedback systems can flag questionable codes and suggest replacements while coders work. Alternatively, machine learning (ML) algorithms can review batches of patient charts post-factum, forwarding clean charts to billing while flagging others for further review. Platforms like IBM Watson demonstrate this potential, enabling organizations like ProSciento to code 84% of terms with a single AI-enabled search. -
Expanding the Role of Medical Coders
The primary beneficiaries are medical coders, who either become “super-coders” capable of handling thousands of codes in seconds or supervisors overseeing complex cases flagged by AI. Additionally, providers can benefit from the advanced capabilities of medical coding AI, such as real-time suggestions while drafting notes, making the coding process even more seamless.
Benefits of AI in Medical Coding
By integrating AI into medical coding, providers can unlock several key advantages:
-
Scalability Without Limits
AI operates 24/7, processing far more patient records than any human team could. This means faster superbill preparation and fewer delays, with the only limitation being the capacity of your cloud provider—which is often highly cost-effective. -
Improved Accuracy and Precision
Machine learning ensures no codes are missed, even those that might slip through the cracks during manual coding. This reduces the risk of under-coding and ensures accurate reimbursement, maximizing revenue. -
Reduced Operational Costs
With AI shouldering a significant portion of the workload, providers can reduce the need for manual coders, reposition staff into supervisory roles, or allocate them to more critical tasks. This also lightens the load on the auditing side, saving even more resources. -
AI as a Training Resource
AI can also serve as an educational resource, helping new coders learn patterns by comparing correct and incorrect coding instances. Over time, this improves staff efficiency and ensures best practices are consistently followed.
Have a Project Idea in Mind?
Get in touch with experts for a free consultation. We’ll help you decide on next steps, explain how the development process is organized, and provide you with a free project estimate.
AI in Medical Billing
AI in medical billing is revolutionizing workflows and addressing some of the most persistent challenges in the industry. By leveraging advanced algorithms and machine learning, providers can achieve faster, more accurate, and efficient billing outcomes.
Smarter Data Processing
AI medical billing software is exceptionally good at processing and recognizing critical billing data. From insurance cards to health records and other digitally captured texts, AI uses natural language processing (NLP) enhanced by neural networks to handle this information. What’s more? It doesn’t just stop at recognition. AI can identify patterns in successful claims and predict risks for rejected ones. This means healthcare providers can proactively address potential issues before claims are even submitted.
How AI Improves Billing Workflows
AI is a game-changer for billers, simplifying their workflows in several impactful ways:
-
Insurance Eligibility Validation
Forget the manual back-and-forth of verifying insurance details. AI in medical billing handles this process quickly and accurately, ensuring claims are submitted with the correct information from the start.
-
Claims Submission and Tracking
AI doesn’t just automate claims submission—it also keeps an eye on them during the review process, flagging potential problems and tracking progress. -
Learning from Rejections
AI can be trained on previously rejected claims to predict future risks. By flagging risky claims before submission, it helps billers reduce denials and improve approval rates. -
Streamlined Patient Onboarding
AI recognizes patient IDs and ensures accurate data entry into health records. This reduces errors during onboarding and saves time for both patients and staff. -
Prioritizing Tasks
Not all tasks are created equal, and AI knows this. By ranking tasks based on their impact on revenue, AI ensures that billers focus on what matters most, helping providers maximize their bottom line.
And for a futuristic twist? Voice-enabled data input could allow billers to capture information hands-free, adding even more efficiency to the process.
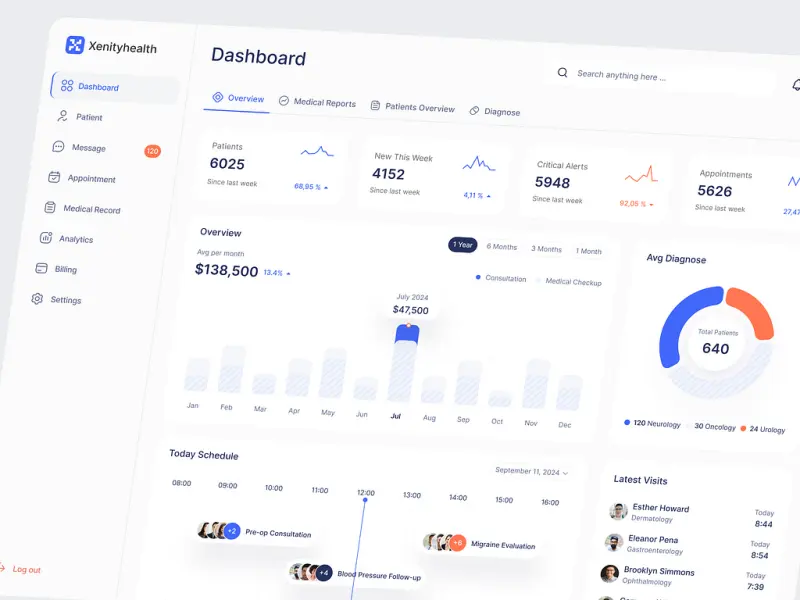
Benefits of AI in medical billing
Who Benefits from AI-Powered Billing?
AI’s benefits extend beyond just billers. While it primarily supports their workflows, insurance carriers also stand to gain by processing approvals and denials faster. This creates a smoother, more efficient ecosystem that benefits everyone involved in the claims process.
The Benefits of AI in Medical Billing
AI-driven medical billing delivers a host of benefits that make life easier for healthcare providers:
- More Approved Claims: AI reduces errors and ensures claims are accurate, leading to fewer rejections.
- Higher Revenue: With precise code attribution, providers maximize reimbursements without leaving money on the table.
- Lower Operating Costs: Automation reduces the need for manual input, freeing up resources for other priorities.
- Less Burnout: By taking on repetitive tasks, AI helps ease the workload for billers, allowing them to focus on more meaningful work.
In short, AI doesn’t replace billers—it empowers them. By automating the heavy lifting, billers can step into supervisory roles, focusing on oversight and resolving complex cases.
III. Challenges in Implementing AI for Billing and Coding
While AI in medical billing and coding offers immense potential, implementing it isn’t without its hurdles.
AI in medical billing
Here’s what healthcare organizations should keep in mind:
- Navigating HIPAA Compliance
When handling sensitive patient data, compliance with HIPAA regulations is non-negotiable. AI systems must be secure and meet strict standards to protect financial and health information. - Addressing Data Format Variability
Let’s face it: not all systems play well together. Many organizations still use outdated software that outputs data in incompatible formats. To maximize AI’s potential, seamless integration with third-party tools and platforms is essential. - Ensuring Integration with Insurance Carriers
For claims to flow smoothly, insurance carriers must support the same infrastructure. Providers can either integrate their AI systems with carriers’ APIs or offer their own tools to streamline data exchange. - Overcoming Staff Pushback
It’s natural for billers and coders to feel concerned about AI taking over their roles. But here’s the truth: AI isn’t here to replace them—it’s here to help. Educating staff on how AI enhances their workflows and lightens their workload is key to successful adoption. - Training AI with Quality Data
Super-smart AI systems don’t appear out of thin air—they need robust data to learn. Access to historical claims, including both approved and rejected ones, is critical for training algorithms to perform at their best. - Adapting to Evolving Standards
The switch from ICD-10 to ICD-11, which began in January 2022, highlights the need for continuous adaptation. AI systems must stay updated to handle new codes and standards as the industry evolves.
IV. The Future of AI in Healthcare Billing and Coding
AI in medical billing is set to redefine how healthcare billing is done, and the future looks incredibly promising. With advancements in technology, deeper integrations with healthcare systems, and widespread adoption, AI could transform not just billing but how the entire healthcare industry operates. Let’s break down what’s on the horizon.
The technology behind AI in medical billing is evolving fast, and it’s only getting smarter. Here’s what we can expect:
-
Smarter Machine Learning Algorithms
Machine learning is the backbone of AI, and it’s improving every day. Future algorithms will better understand complex billing scenarios, predict claim denials with greater accuracy, and even recommend ways to fix errors in real time. -
Improved Natural Language Processing (NLP)
NLP is what allows AI to understand human language in documents like doctor’s notes, insurance forms, and health records. As NLP gets better, AI will be able to interpret more nuanced medical terminology, making billing and coding even more precise. -
Handling Complex Medical Coding Situations
With ongoing improvements, AI will be able to tackle complicated coding scenarios that currently require human expertise. Think multiple diagnoses, overlapping treatments, or rare procedures—AI will streamline these situations, reducing the burden on coders and billers.
These advancements mean AI will continue to become a more reliable and indispensable tool for healthcare billing teams.
Conclusion
AI is no longer a futuristic concept—it’s a practical tool that’s transforming medical billing and coding. By automating tedious tasks, improving coding accuracy, and streamlining workflows, AI in medical billing empowers healthcare providers to achieve faster reimbursements, fewer denials, and a more efficient revenue cycle. The benefits are clear: higher revenue, reduced workload, and less stress for your team. TECHVIFY specializes in developing tailored AI solutions designed to meet your billing and coding needs. Contact us for a free consultation to see how we can help streamline your revenue cycle and maximize your results.
TECHVIFY – Global AI & Software Solutions Company
From Startups to Industry Leaders: TECHVIFY prioritizes results, not just deliverables. Accelerate your time to market and see ROI early with high-performing teams, AI (including GenAI) Software Solutions, and ODC (Offshore Development Center) services.
- Email: [email protected]
- Phone: (+84)24.77762.666