Legacy Systems in Healthcare: 6 Steps to a Seamless Upgrade and Better Patient Care
- TECHVIFY Team
- 0 Comments
In recent years, industries across the globe have undergone full-scale digital transformations, and the healthcare sector is no exception. What was once a field dominated by paper forms, manual data entry, and sluggish information exchanges has now evolved into a landscape of telehealth, wearable health trackers, cloud-based data storage, and robust cybersecurity programs. However, despite the rapid technological advancements, not all transformations have been smooth. In fact, only 30% of organizations have reported successful digital transformation projects post-COVID-19. A key determinant of success? The status of their legacy systems.
In this blog, we’ll explore the different types of legacy systems in healthcare, how they impact a healthcare facility’s digital transformation efforts, and the current trends challenging these systems.
I. The Need for Legacy Systems in Healthcare
When we talk about legacy systems in healthcare, we’re referring to software that’s no longer getting updates or improvements from the original vendor. While these systems still handle basic tasks, they remain stuck in their original state without any new developments. Interestingly, despite being outdated, more than 70% of Fortune 500 companies still rely on legacy systems, showing how widespread they continue to be.
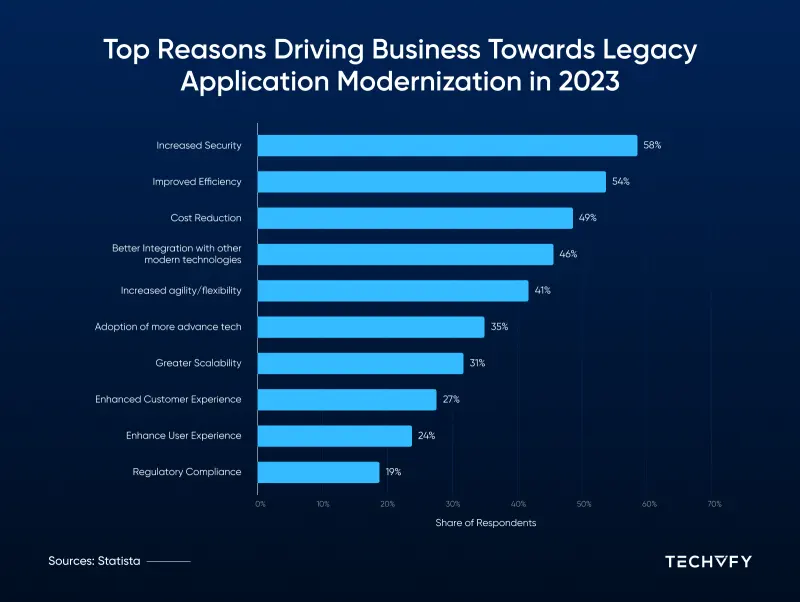
Legacy Healthcare System Market Report
According to Statista, in 2023, most organizations surveyed are focusing on updating their outdated applications and data infrastructures. Over 50% of respondents pointed to better efficiency and security as the main drivers for upgrading. About half also mentioned that reducing costs, improving integration with modern technologies, and gaining more agility were key reasons for making the switch.
A clear case of legacy systems in healthcare is the continued use of outdated electronic health record (EHR) systems. These older systems often have clunky user interfaces, poor compatibility with other tools, and are vulnerable to security threats. When a system lacks modern features like scalability, advanced data analytics, and AI capabilities, it becomes more costly to maintain and hinders improvements in patient care and overall efficiency.
To understand why upgrading is crucial, let’s take a look at the different types of legacy systems in healthcare. Each of these systems needs to be modernized to keep up with the latest technology and ensure smooth operations.
II. Different Types of Legacy Healthcare Systems
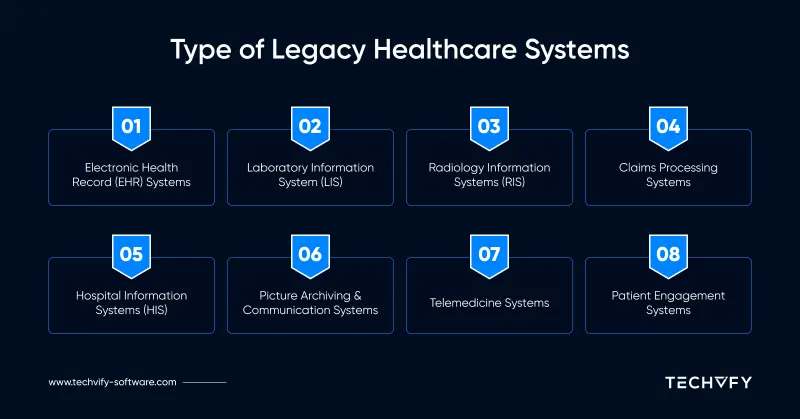
Various healthcare software that once supported essential functions now fall under the category of legacy systems. Let’s explore some of the most common types:
1. Early Electronic Health Record (EHR) Systems
Older versions of EHR systems were designed to handle basic patient records, but over time, they’ve fallen behind in terms of functionality. These older systems often lack the advanced features, ease of use, and interoperability that newer EHR systems offer.
2. Hospital Information Systems (HIS)
Legacy HIS software manages different administrative, financial, and clinical tasks within hospitals. However, outdated HIS can struggle with integrating new tools, providing real-time data access, and generating modern reports.
3. Laboratory Information Systems (LIS)
Legacy LIS handle lab workflows and test results but may face issues with standardizing data and integrating with newer diagnostic technologies.
4. Picture Archiving and Communication Systems (PACS)
These systems are used to store and retrieve medical images. Older PACS may have trouble keeping up with modern imaging technologies and integrating with newer systems.
5. Radiology Information Systems (RIS)
Legacy RIS oversees radiology workflows, such as imaging schedules and billing. Older versions might lack features like automated appointment scheduling and may not integrate well with newer RIS systems.
6. Telemedicine Systems
Outdated telemedicine platforms fall under legacy systems that face challenges in keeping up with the requirements of modern healthcare. These systems need to be upgraded to ensure secure communication and effective telehealth services.
7. Claims Processing Systems
These systems manage the billing and reimbursement process between healthcare providers and insurance companies. Legacy claims processing systems struggle with the complexities of modern billing rules and regulatory requirements.
8. Patient Engagement Systems
Older patient engagement systems often lack the user-friendliness and capabilities of newer solutions. Upgrading these systems is essential for encouraging patients to participate actively in managing their own health.
Type of legacy systems in healthcare
III. Proven Strategies for Upgrading Legacy Medical Systems
Upgrading outdated healthcare systems requires strategic planning to bring them in line with current industry standards and technological advancements. Below are some of the most effective methods for modernizing legacy medical systems:
Conduct a Thorough System Assessment
Start by analyzing your current legacy systems in detail. Evaluate their reliability, functionality, and how they handle data. Document all specifications and set clear objectives for integration, keeping security and scalability at the forefront.
Define Clear Integration Objectives
Clearly define the objectives you intend to accomplish with the upgrade—whether that’s improving data flow, boosting functionality, or ensuring compatibility with modern technologies. These objectives need to be in sync with the larger goals of your organization to ensure the project’s success contributes to long-term growth.
Select the Best Integration Approach
Based on your assessment and existing infrastructure, choose an integration strategy that works best for your needs—whether it’s data migration, APIs, middleware, or a combination. Ensure the selected method can scale and adapt to your organization’s future requirements.
Implement Middleware for Smooth Communication
Middleware can serve as a bridge between old and new systems. Ensure the middleware is set up to allow seamless data transfer and system interoperability without causing operational disruptions.
Leverage API Integration
If you’re using APIs, make sure they’re designed to work with both legacy and modern applications. Safeguard sensitive information by implementing proper authorization and authentication protocols during the integration process.
Plan a Comprehensive Data Migration
During the process of transferring data from older systems to new environments, plan the process carefully to avoid mistakes. Maintain data accuracy and uniformity during the entire migration process to maintain the system’s integrity.
Conduct Rigorous Testing
Before fully integrating the new systems, carry out extensive testing. This includes user acceptance testing, unit testing, and integration testing to identify and address any issues that could hinder functionality.
Use a Phased Rollout for Implementation
To avoid disrupting daily operations, adopt a phased approach to rolling out the new system. This allows you to monitor the process closely and quickly resolve any issues that may arise.
Maintain Continuous Monitoring and Improvement
Once the new system is live, monitoring tools will be used to track performance and gather user feedback. Regularly update and optimize the system to keep up with changing business needs and improve the user experience.
By following these strategies, healthcare organizations can modernize legacy systems and create a more agile, efficient technology infrastructure that keeps pace with the changing needs of the healthcare industry.
Looking to Outsource Development?
Contact TECHVIFY – Vietnam’s Leading Offshore Software Development & Outsourcing Company, for consultation and development services.
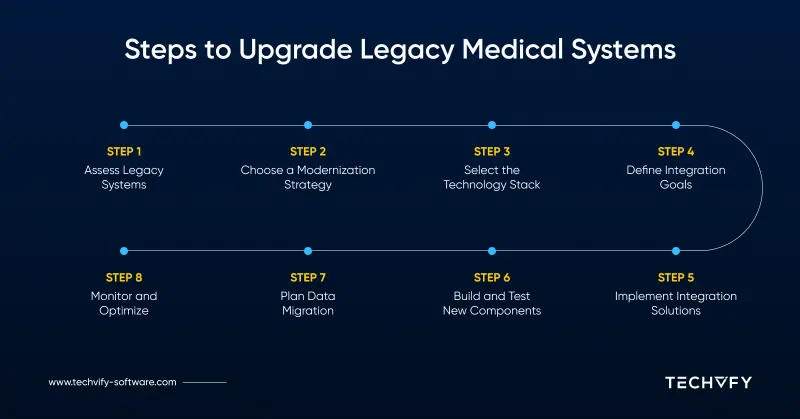
IV. Breakdown The Guide to Modernizing Healthcare Systems
Modernizing healthcare IT systems is a multifaceted process requiring thorough planning, careful execution, and constant monitoring. Every step is essential to achieving a successful result. Below are the detailed steps involved in modernizing legacy healthcare IT systems, from the initial evaluation to post-modernization optimization.
Legacy systems healthcare – Upgrade guide
Step 1: Conduct a Comprehensive Assessment of Legacy Systems
The first step in modernizing healthcare IT systems is conducting a full-scale audit of the existing infrastructure. This involves identifying all hardware, software, and systems currently in use. Evaluate their age, performance metrics, compatibility, and any potential security vulnerabilities. It’s also essential to gather feedback from key stakeholders, including end-users (such as healthcare providers), IT staff, and executive leadership, to understand their concerns and expectations.
In addition to performance analysis, assess the total cost of ownership, including maintenance, support, and downtime costs. This will give the organization a clear picture of the financial implications of maintaining legacy systems versus modernizing them.
Once the audit is complete, prioritize mission-critical systems according to their influence on patient care and operational effectiveness, and compliance with healthcare regulations like HIPAA. Finally, prepare a detailed report that outlines the findings, risks, and recommended phased modernization approach.
Step 2: Select the Most Appropriate Modernization Approach
Choosing the right modernization approach is crucial for a successful transition. Consider the following strategies:
- Rehosting: Move the application to the cloud with minimal changes. This is a quick solution but doesn’t address deeper architectural issues or leverage cloud-native features.
- Refactoring: Modify the application code to improve performance and compatibility without altering the overall architecture.
- Rearchitecting: Redesign the application’s architecture to modern standards, improving scalability and modularity. This requires more effort but results in a more future-proof system.
- Rebuilding: Create a new, modern version of the application from scratch. This is a costlier and time-consuming approach but is necessary if the legacy system is no longer viable.
- Replacing: Implement a new off-the-shelf solution to replace the legacy system. This requires careful evaluation to ensure that the new system meets all the organization’s requirements, including data migration.
Evaluate the feasibility, cost, and timeline of each approach by considering the complexity of the legacy system, its role in patient care, and its impact on clinical workflows. Ensure that the chosen approach aligns with the organization’s long-term goals and regulatory requirements, such as HIPAA and HL7 standards.
Step 3: Choose the Optimal Technology Stack for Modernization
Modernizing healthcare IT systems requires selecting appropriate technologies that are scalable, secure, and compliant with healthcare regulations. Begin by evaluating cloud platforms like AWS, Google Cloud, or Microsoft Azure, which offer robust security features, interoperability, and scalability.
Next, consider adopting modern healthcare solutions, such as cloud-based Electronic Health Record (EHR) systems like Cerner or Epic, which are capable of managing substantial amounts of patient data and integrating seamlessly with other healthcare systems. Prioritize compliance with healthcare regulations, ensuring chosen technologies support HIPAA-compliant data storage and secure communication protocols like HL7 FHIR.
For more advanced data security, consider integrating blockchain technology for secure data sharing and auditing. Lastly, ensure that the technology stack aligns with the organization’s long-term goals and budget. If developing a mobile health app, frameworks like React Native or Flutter offer robust ecosystems with healthcare-specific libraries and cross-platform capabilities.
Step 4: Set Clear Integration Goals for the Modernized System
Defining integration goals ensures that IT modernization aligns with the organization’s strategic vision. Here are key integration goals healthcare organizations should consider:
- Real-Time Data Access: Ensure patient data is accessible in real-time across different departments.
- Secure Medical Record Sharing: Facilitate secure sharing of patient records with external providers and third-party systems.
- Interoperability: Enable seamless communication between legacy systems and emerging technologies, such as wearables, remote monitoring devices, and artificial intelligence tools.
- Administrative Efficiency: Streamline administrative processes by integrating billing, scheduling, and inventory management systems.
To prioritize integration goals, begin by identifying the challenges posed by current legacy systems, such as data silos or inefficiencies in data sharing. Ensure compliance and data security are top priorities, given the importance of protecting patient information. Conduct a cost-benefit evaluation to assess the practicality of each integration goal and its potential impact on the healthcare organization.
Step 5: Select an Integration Method and Implement Middleware Solutions
The choice of integration method is crucial to facilitating smooth communication between outdated and current systems. Below are common integration methods for healthcare systems:
| Integration Method | Use Cases | Examples |
|---|---|---|
| Enterprise Service Bus (ESB) | Integrate multiple applications across the organization, enabling data orchestration | Integrating EHR with billing, lab, and clinical decision support systems |
| Point-to-Point (P2P) | Directly connect two systems for simple integrations | Integrating a medical device with an EHR system for real-time data transfer |
| API Integration | Use APIs to enable data exchange and integration between systems | Integrating a telemedicine platform with EHR for remote access to patient data |
| Robotic Process Automation (RPA) | Automate repetitive tasks, especially for legacy systems with limited integration | Automating data extraction from a legacy system to a modern EHR system |
| Integration Platform as a Service (IPaaS) | Cloud-based integration platform for rapid deployment and reduced infrastructure needs | Integrating cloud-based healthcare apps with on-premises systems like EHR and practice management |
To implement middleware solutions:
- Begin by assessing system requirements, including data formats, security protocols, and performance needs.
- Select the middleware solution that best meets your integration goals.
- Establish data mappings and transformations to guarantee smooth data flow between systems.
- Implement security measures, such as data encryption and access controls, to protect sensitive healthcare information.
- Carry out comprehensive tests to confirm the functionality and efficiency of the middleware solution.
- Deploy the middleware and monitor its performance for any emerging issues.
- Provide training to end-users and support teams to ensure a smooth transition and continuous maintenance.
Step 6: Develop and Test Modern Components of the System
Developing and testing modern system components is a critical phase in the modernization process. Follow these steps to ensure success:
- Requirement Gathering: Collaborate with healthcare professionals, IT teams, and other stakeholders to define system requirements.
- Agile Development: Use an iterative development approach to build and test system components in small increments.
- Cross-Functional Teams: Establish teams of developers, quality assurance specialists, and subject matter experts to foster collaboration and continuous improvement.
During development, conduct comprehensive testing to ensure the system meets healthcare-specific requirements:
- Usability Testing: Ensure that the system’s user interface is intuitive for healthcare professionals.
- User Acceptance Testing (UAT): Gather feedback from real healthcare workers to refine the system based on their needs.
- Performance Testing: Test the system’s ability to handle peak workloads and large volumes of data without performance degradation.
- Security Testing: Ensure that the system complies with healthcare regulations like HIPAA by testing encryption, access controls, and vulnerability management.
- Integration Testing: Verify that the system integrates seamlessly with other medical systems, including laboratory information systems or third-party applications.
Step 7: Execute a Detailed Data Migration Strategy
Data migration is a complex process that requires proper planning and execution. Here’s how to carry out effective data migration:
- Data Profiling and Cleansing: Begin by identifying and addressing any inconsistencies, duplicates, or errors in the legacy data.
- Define Data Models and Schemas: Design the data models and schemas required for the modernized system, aligning them with organizational and regulatory requirements.
- ETL Process: Execute the Extract, Transform, and Load (ETL) procedure to transfer data from the old system to the new platform. Use specialized tools or scripts for automated data migration.
- Data Validation and Reconciliation: Thoroughly test the migrated data to verify its integrity, accuracy, and completeness. Resolve any discrepancies between the legacy and modernized systems.
- Stakeholder Communication: Maintain regular communication with stakeholders, documenting any challenges that arise and monitoring the migration process closely.
Step 8: Implement Continuous Monitoring and Optimization for the Modernized System
After the successful implementation of the modernized system, continuous monitoring is essential to ensure smooth operations and optimal performance. Here’s how to manage monitoring and optimization:
- Define Monitoring Objectives: Identify which aspects of the system require monitoring, such as application performance, security events, and compliance requirements.
- Establish Key Performance Indicators (KPIs): Identify KPIs such as response time, resource utilization, error rates, and security incidents.
- Deploy Monitoring Tools: Use appropriate monitoring tools such as Splunk, Nagios, Zabbix, SolarWinds, or AppDynamics to track system performance and detect issues.
- Set Alerts and Notifications: Configure alerts for KPIs that breach predefined thresholds, ensuring that IT staff is notified of potential problems.
- Analyze and Optimize: Regularly review monitoring data to identify performance bottlenecks and implement optimizations to enhance system efficiency and security.
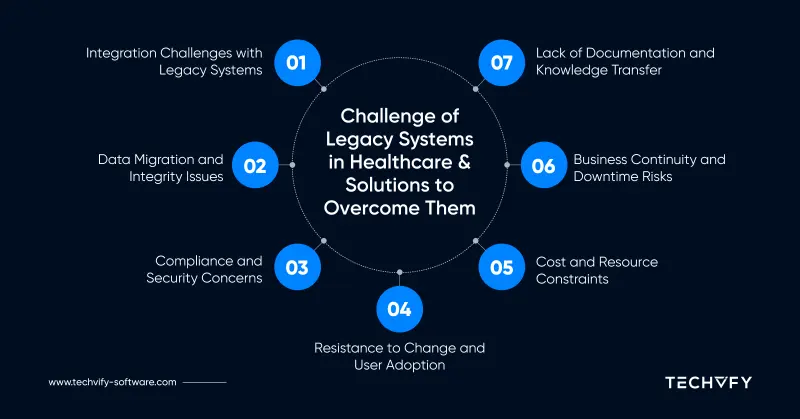
V. Key Challenges Faced During Healthcare IT System Modernization
Modernizing legacy systems in healthcare is a complex process involving technological, operational, and regulatory challenges. This transformation affects a wide range of stakeholders, including healthcare providers, patients, and regulatory bodies. Below are the major challenges healthcare organizations face when undertaking IT modernization initiatives.
Challenges of legacy systems in healthcare
Difficulty in Integrating Modern Technologies with Legacy Systems
One of the primary challenges of modernizing healthcare IT systems is integrating new technologies with outdated legacy systems. These older systems often rely on outdated architectures and programming languages, making seamless integration with modern software and hardware solutions difficult.
Legacy systems tend to create isolated “data silos” where critical patient information is stored separately, making it hard to achieve interoperability across departments or with external systems. As a result, healthcare organizations often face inefficiencies in workflow, leading to delays in patient care and increased operational costs. Addressing this challenge requires careful planning and selecting integration approaches that can connect the gap between old and new technologies.
Challenges in Data Migration and Ensuring Data Integrity
Migrating years—sometimes decades—of patient data from legacy systems to modern platforms is a significant undertaking. Healthcare organizations must ensure that data is not only transferred completely but also accurately.
Data migration poses risks such as incomplete transfers, data corruption, and potential loss of critical patient information. Any compromises in data integrity can jeopardize patient care, potentially leading to legal risks for the organization. Ensuring that the migrated data is both accurate and compliant with healthcare regulations is critical, which requires rigorous testing and validation throughout the migration process.
Regulatory Compliance and Data Security Concerns
The healthcare sector operates under stringent regulatory requirements, particularly concerning data security and patient privacy. In the United States, regulations like HIPAA (Health Insurance Portability and Accountability Act) enforce strict rules on how healthcare organizations manage, store, and share patient data.
Modernizing legacy systems involves ensuring that all new platforms and processes adhere to these regulations. Failure to comply can result in severe penalties, including substantial fines and reputational damage. Moreover, maintaining data security during the transition from old to new systems is critical, as healthcare data breaches are costly and can severely affect patient trust.
Overcoming Resistance to Change and Ensuring User Adoption
One of the most overlooked challenges in healthcare IT modernization is change management. Healthcare professionals are accustomed to using established workflows and systems, and introducing new technologies can create resistance among staff.
Adopting new systems often requires healthcare providers and support staff to undergo extensive training. Without sufficient training and support, staff may struggle to adapt to new workflows, leading to inefficiencies and frustration. Successful modernization requires clear communication, ongoing training, and stakeholder engagement to ensure that all users are comfortable with the new systems.
Managing Costs and Resource Limitations
Modernizing legacy systems is not only a technical challenge but also a financial one. Healthcare organizations often operate under tight budgets, making it difficult to secure the necessary funds for system upgrades, new infrastructure, and training programs.
In addition to financial constraints, there is often a shortage of skilled IT professionals who have expertise in both legacy and modern systems. This scarcity can delay modernization efforts, further increasing costs and extending timelines. To address these challenges, organizations must carefully budget for modernization and invest in acquiring or training the necessary talent to support the transition.
Ensuring Business Continuity and Minimizing Downtime
Healthcare operations are highly sensitive to system downtimes, as even short periods of unavailability can have serious consequences for patient care. During the modernization process, organizations must ensure that critical services remain operational.
Ensuring business continuity requires careful planning to minimize disruptions during system transitions. This includes having contingency plans, such as backup systems, and implementing robust disaster recovery strategies. Without proper planning, system downtime can lead to delayed treatments, compromised patient safety, and increased workloads for healthcare staff.
Overcoming the Lack of Legacy System Documentation and Knowledge Transfer
Legacy systems often suffer from poor or incomplete documentation, making it difficult for modernization teams to fully understand how the systems operate. Moreover, the knowledge of these systems is frequently concentrated in a few individuals, many of whom may be nearing retirement.
The lack of documentation and the reliance on a small group of experts pose significant risks to modernization efforts. Transferring institutional knowledge from legacy system experts to modernization teams requires proactive knowledge management strategies. Organizations should focus on documenting existing systems thoroughly and ensuring that critical knowledge is shared with modernization teams before key personnel retire or move on.
Conclusion
Modernizing legacy systems in healthcare is no longer just an option—it’s a necessity. The digital transformation of healthcare, driven by advances in telehealth, cloud-based data storage, and cybersecurity, offers significant potential to improve patient care, operational efficiency, and data security. However, as we’ve discussed, the barriers to successful modernization—ranging from data migration to regulatory compliance—are formidable.
Contact TECHVIFY for expert consultation and development services. We’ll help you modernize your IT infrastructure, ensuring better efficiency, security, and scalability—while minimizing disruption to your operations.
Get in touch with TECHVIFY today and see how we can help you transform your legacy systems into modern, high-performing solutions.
TECHVIFY – Global AI & Software Solutions Company
For MVPs and Market Leaders: TECHVIFY prioritizes results, not just deliverables. Reduce time to market & see ROI early with high-performing Teams & Software Solutions.
- Email: [email protected]
- Phone: (+84)24.77762.666